Past Issues
Establishing Physician-Governed Social Media Accreditation to Combat the Spread of Misinformation by Non-Medical Skinfluencers
Nicole Werpachowski1, Olumayowa Adebiyi2, Neena Edupuganti3, Kasey Smith4, Grace Herrick5, Avva Saniee6, Kelly Frasier7*, Alina G Bridges7
1Department of Medicine, Lenox Hill Hospital, Northwell Health, New York, NY, USA
2Department of Internal Medicine, St. John’s Riverside Hospital, Yonkers, NY, USA
3Department of Medicine, Piedmont Healthcare, Macon, GA, USA
4Department of Medicine, HCA Florida Blake Hospital, Bradenton, FL, USA
5Alabama College of Osteopathic Medicine, Dothan, AL, USA
6Department of Medicine, Memorial Healthcare System, Pembroke Pines, FL, USA
7Department of Dermatology, Northwell Health, New Hyde Park, NY, USA
*Corresponding author: Kelly Frasier, DO, MS, Department of Dermatology, Northwell Health, New Hyde Park, NY, United States, Phone: 3105956882, Email: [email protected]
Received Date: July 14, 2025
Publication Date: September 09, 2025
Citation: Werpachowski N, et al. (2025). Establishing Physician-Governed Social Media Accreditation to Combat the Spread of Misinformation by Non-Medical Skinfluencers. Dermis. 5(5):49.
Copyright: Werpachowski N, et al. © (2025).
ABSTRACT
Implementing physician-governed social media accreditation represents a potential strategy to address the widespread misinformation spread by non-medical skinfluencers and to restore trust in online dermatologic advice. While social media platforms serve as a primary source of skincare information for millions online, unqualified individuals lacking formal medical training can influence public health by disseminating unverified, misleading, or even harmful practices. This unchecked flow of misinformation threatens public health by promoting unsafe skincare practices and perpetuating widespread misconceptions. A well-structured physician-governed accreditation system could establish standards for content creators, ensuring that all skincare advice shared online is evidence-based, scientifically sound, and medically responsible. This literature review synthesizes existing evidence on dermatology-related misinformation and considers a physician-led accreditation system as a potential response to addressing existing gaps in digital health oversight. An accreditation model could help provide the public with clearer ways to distinguish reliable sources from misinformation, promoting safer dermatologic practices online. Furthermore, accreditation would mandate ongoing dermatologic education, disclosure regarding conflicts of interest, and the use of real-time monitoring tools to flag and correct misleading content. This proposed framework also underscores how dermatologists may strengthen their role as visible authorities in the digital space while ensuring that communication online regarding skincare and dermatology remains ethical and evidence-driven. By addressing gaps in oversight, physician-governed accreditation could protect consumers by reducing misinformation, expanding access to accurate information, and shaping standards for responsible, evidence-based dermatologic communication in the digital age.
Keywords: Dermatology, Social Media, Health Misinformation, Accreditation, Digital Health Policy
INTRODUCTION
Social media has become a prevailing force in shaping dermatology-related behaviors, where visually appealing content lends itself to mass digital engagement. The emergence of “skinfluencers,” or social media personalities who offer skincare advice or endorse dermatologic products, has given rise to a parallel ecosystem of dermatologic information that is often unregulated, commercialized, and devoid of clinical oversight. Although some skinfluencers offer practical insights based on personal experience, many lack any formal medical training, raising concerns about the reliability of the information being circulated. Surveys consistently show that patients use the internet as the first source for dermatologic guidance [1].
The unchecked nature of social media platforms has enabled the viral spread of unverified dermatologic myths and dangerous trends. These practices can exacerbate chronic skin conditions, delay appropriate medical treatment, and lead to long-term consequences. A recent analysis of dermatology-related TikTok videos found that only a small percentage were created by board-certified dermatologists, with the majority produced by non-professionals, including influencers, patients, and businesses. This content from non-physicians garnered significantly higher engagement, emphasizing the power of popular, yet potentially inaccurate, messaging in shaping public understanding of skin health [2]. Despite the risks, algorithm-driven content amplification often favors entertainment and virality over credibility, allowing non-evidence-based content to reach vast audiences [3]. As dermatologists observe the growing influence of non-medical voices online, there is an increasing call for interventions to safeguard public health and promote accurate education.
Professional organizations have begun to address these challenges. For example, the American Academy of Dermatology launched the "Your Dermatologist Knows" campaign, a consumer-focused initiative that successfully amplified physician-created content across social media [4]. However, such initiatives are primarily promotional and do not provide a mechanism to formally verify content accuracy, flag misinformation, or hold non-medical influencers accountable. While platforms like YouTube and TikTok offer opportunities for outreach, their open-access nature leaves audiences vulnerable to misinformation without expert oversight. No established system of content regulation currently exists that enables consumers to distinguish between credible sources and potentially harmful advice. A physician-led social media accreditation model could fill this gap by establishing enforceable standards for digital skincare content, ensuring ongoing professional oversight, and offering the public a transparent way to identify trustworthy dermatology information. This literature review outlines the scope of dermatology-related misinformation, limitations of current verification countermeasures, and a conceptual framework for a physician-governed accreditation model as a potential approach to strengthen accountability, transparency, and evidence-based standards in digital dermatologic communication.
REVIEW
Scope of Dermatologic Misinformation on Social Media
Social media platforms have become primary sources of dermatology-related health information, allowing for the rapid spread of dermatology-related misinformation. Common misinformation trends include “natural” or “do it yourself” (DIY) remedies (e.g., applying lemon juice or toothpaste to the skin), exaggerated concerns around dermatologist-recommended products like sunscreens and retinoids, and endorsement of devices or regimens lacking FDA oversight. Persistent myths, such as acne being caused by poor hygiene or sun exposure, continue to influence patient behavior despite robust supporting evidence vastly debunking these claims [5]. Such misinformation encourages harmful practices, such as excessive cleansing, dietary restriction, or unsafe sun exposure. Additionally, misinformation surrounding topical corticosteroid use, particularly “topical steroid withdrawal” narratives, has spread widely on TikTok and Instagram, reinforcing unfounded fears and reducing treatment adherence among individuals with chronic skin conditions [6]. Given the viral nature of digital content and the high engagement it generates, dermatologists face increasing pressure to actively address evidence-based skincare communication and counter false narratives to protect public health.
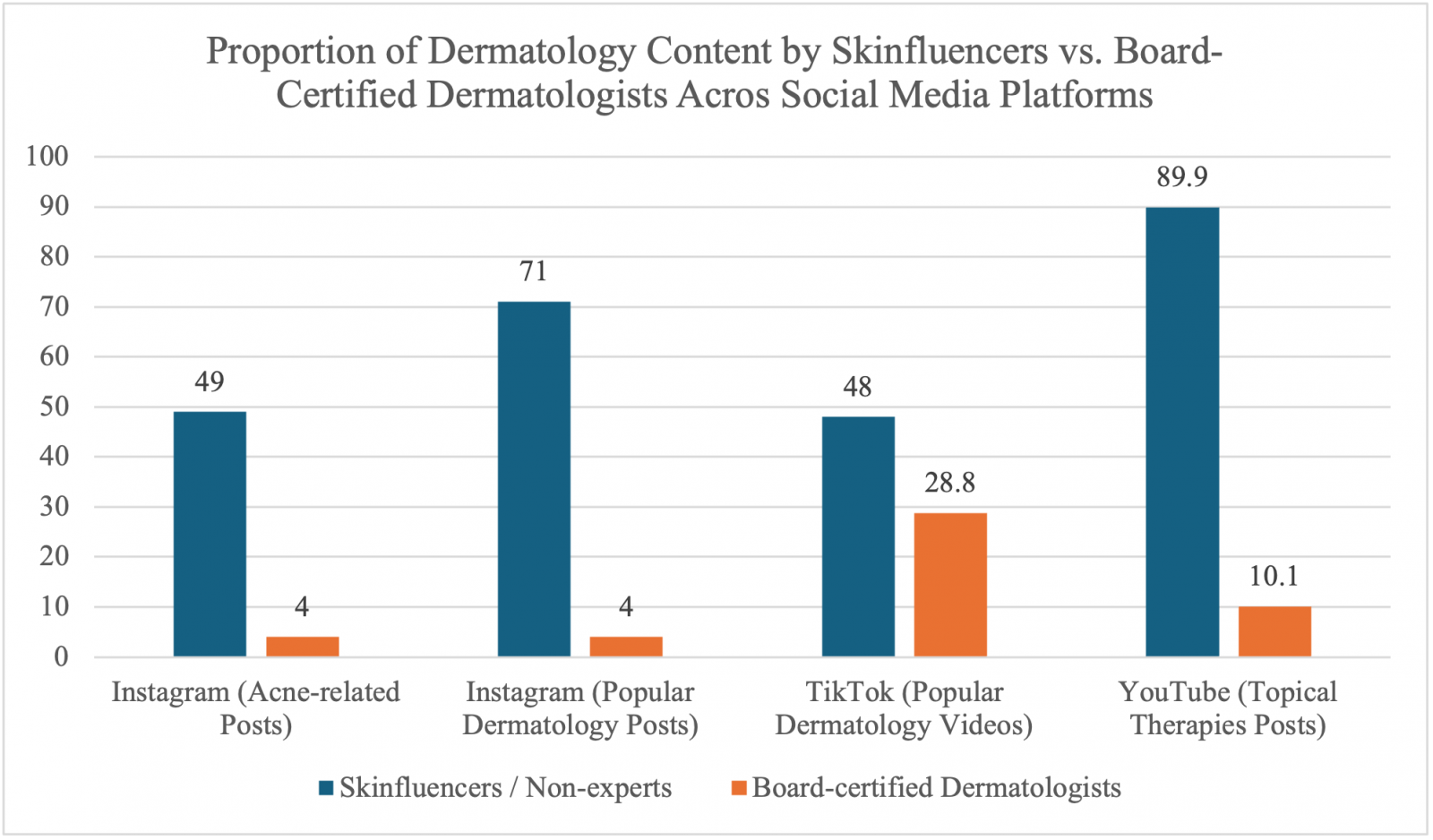
Multiple studies confirm the prevalence and scope of dermatology misinformation across online platforms, particularly among non-expert social media influencers (Figure 1). On Instagram, for example, over 59% of top acne-related posts were created by influencers, while fewer than 4% originated from board-certified dermatologists. Among these treatment-related posts, only 11% referenced grade some therapies as outlined by the American Academy of Dermatology (AAD) guidelines [7]. Similarly, another study found that 45% of acne patients consulted social media for acne treatment advice, yet only 31% implemented changes that were in alignment with the American Academy of Dermatology’s (AAD) clinical guidelines [8]. A separate 2020 cross-sectional study analyzing the most popular dermatology-related posts on Instagram found that only 4% of influencers were board-certified dermatologists. In contrast, approximately 71% did not list any formal medical credentials [9]. Similar findings were revealed on TikTok, whereby one study found 48% of popular dermatology videos were created by patients, while only 25.8% originated from board-certified dermatologists [10]. Notably, dermatologist-created educational videos adhered to AAD guidelines with 96.8% reliability, compared to the 48% accuracy rate among those posted by patients [10]. Similarly, another study evaluating information about topical psoriasis therapies on YouTube found that only 10.1% of videos featured healthcare professionals, whereby videos that discussed critique or negative experiences with medically-prescribed therapies had significantly more views and engagement [11]. Yet, this widespread lack of verified expertise is further complicated by the fact that a majority of these accounts included promotional or self-promotional content, introducing potential conflicts of interest that may prioritize monetization over the integrity of the content.
Figure 1. Proportion of dermatology content created by non-experts and board-certified dermatologists across various social media platforms.
Compounding this issue, engagement-driven algorithms amplify and reward content designed for entertainment and visual appeal rather than clinical accuracy. As a result, dermatology-related misinformation often outperforms expert-guided content in both reach and influence. A cross-sectional analysis revealed that fewer than 35.3% of dermatology content was found to be medically precise, yet imprecise skin health content consistently generated greater engagement than medically accurate content, raising concerns about the feedback loop that amplifies and rewards misinformation [12]. This rise of engagement-driven algorithms has further fueled the dominance of non-medical skinfluencers within dermatology digital discourse. A scoping review by Kaňková et al. described how social media influencers curate content optimized for audience engagement using emotional language, interactive features, and consistent branding, fostering parasocial bonds and perceived credibility among followers even in the absence of formal medical training [13]. Within dermatology, as health communication becomes increasingly commercialized, skinfluencers are incentivized to produce content that aligns with consumer market trends, facilitating the promotion of pseudoscientific routines, unregulated devices, and aesthetic procedures. This blurring between education and advertisement undermines dermatologists' authority in public health conversations, reflecting a systemic failure to prioritize medical validity on social media platforms.
Limitations of Existing Efforts
Social media platforms have implemented various standard tools such as community guidelines, reporting systems, algorithm moderation, and third-party fact-checking to address dermatology-related misinformation. However, these measures remain largely reactive, inconsistently enforced, and not well-equipped to detect the more nuanced or ambiguous medical inaccuracies common in dermatology-related misinformation content online. According to the 4 i Framework for Advancing Communication and Trust, institutional approaches like algorithmic regulation and media verification exist but are rarely optimized for health information, resulting in persistent oversight gaps for dermatology content [14]. Compounding this problem is the design of social media platforms themselves, whereby platform algorithms prioritize emotionally engaging or entertaining content over clinically accurate information, frequently amplifying dermatology videos created by non-experts as above [10]. These factors contribute to misinformation that is not only harder to identify but also easier to believe and share.
The influencer economy further complicates dermatology misinformation, as many sponsored endorsements and promotional partnerships are often undisclosed. This makes it even more difficult for audiences to reliably discern commercial promotion from evidence-based advice [15]. Even when misinformation is identified, attempts to report or remove misleading posts through existing content moderation systems are further impeded by moderation teams typically lacking the clinical expertise necessary to evaluate potential dermatologic harm. These limitations reveal critical gaps in existing platform policies and influencer-driven self-regulation, leaving dermatologic misinformation online without consequence.
Rationale for Physician-Governed Social Media Accreditation
Grounded in their professional commitment to protect patient health, physicians have an ethical responsibility to promote accurate health information and actively combat misinformation in public forums. Several professional organizations, including the American Medical Association (AMA) and American Academy of Dermatology AAD), have delineated frameworks that emphasize accuracy, transparency, and confidentiality in digital communication [16-20]. For example, the AMA highlights the influence of physicians’ online presence on public trust, highlighting how physicians should ensure that content shared online is evidence-based, maintains patient confidentiality, and directs audiences to seek appropriate medical care [18]. Similarly, the AAD encourages dermatologists to contribute responsibly to online discourse, supporting physician-led efforts that promote the dissemination of accurate, peer-reviewed content [19,20]. For example, dermatologists who feature sponsored skincare products on TikTok had higher follower counts [21], and products labeled as “dermatologists recommended” are associated with increased consumer sales [22]. Despite these clear mandates by professional organizations, social media platforms offer limited institutional support, hindering effective physician engagement in the digital landscape.
Dermatologists also remain underrepresented on major platforms. One reason is time constraints, as the creation of content itself is time-intensive, yet rarely recognized in traditional academic or clinical performance metrics [23]. Additional concerns about the blurring of personal and professional identities, as well as the risk of being misinterpreted, leading to potential reputational harm, further discourage participation [24,25]. There are also legal and ethical uncertainties concerning patient privacy, consent, and liability, like the use of medical photography or the provision of personalized medical advice online. These further complicate online engagement, especially as current malpractice policies typically don’t have clauses that cover social media communications [26,27]. These challenges are exacerbated by the absence of dermatology-specific verification systems. While verification badges do exist on some platforms, these symbols fail to convey professional credibility or content accuracy, leaving the public unable to distinguish between credible, board-certified physicians and non-medical skinfluencers.
Dermatology and skin-related content is particularly vulnerable because of its inherently visual and anecdotal nature, which appeals to audiences seeking quick solutions or personal validation for their dermatology-related complaints. It is among the most frequently searched medical specialties on social media, drawing interest from both patients and general social media consumers [22]. This visibility makes dermatology both vulnerable to misinformation and uniquely positioned to lead solutions in reclaiming the narrative.
A structured, physician-governed accreditation system would address dermatology-related misinformation and existing limitations and gaps by providing the public with a reliable way of identifying credible, evidence-based content. Dermatologists are particularly suited to lead such efforts, given their clinical expertise in skin health and the public’s strong interest in dermatologic content. The implementation of such a system would strengthen the specialty’s role in guiding digital health communication and literacy, restoring professional oversight by elevating evidence-based voices through credible verification. The next section outlines some key considerations for the development of such a system, reinforcing the role of dermatologists in guiding digital health communication on skin health.
Conceptual Principles for Accreditation Framework
A dermatology-specific accreditation system can draw on lessons from existing models of digital health regulation. For instance, the Health On the Net (HON) Foundation’s HONcode certification set early ethical standards for credibility and transparency of online medical content, setting a precedent for trustworthy digital communication in medicine [28]. In addition, the AAD successfully launched the “Your Dermatologist Knows” campaign to amplify dermatologist-created content across social media platforms. In 2024, the campaign achieved over 11,600 media placements in outlets, including The New York Times and The Washington Post, and across social media platforms like Instagram and TikTok, generating 125.2 million impressions and 20.4 million engagements [4]. This initiative effectively disseminated accurate, dermatologist-approved information to counter widespread myths and unsafe practices circulating online. Despite this campaign’s success, it did not provide a mechanism or solution to formally verify content accuracy, flag misinformation, or hold non-medical influencers accountable. Considerations such as clear governance, sustainable funding, robust auditing mechanisms, transparency, and addressing physician barriers are necessary for the practical implementation of this system, which will be discussed below.
Existing research on social media behavior consistently shows that users are more likely to engage with influencers perceived as credible and knowledgeable [29]. This trend has been particularly evident in the fitness sector. A 2024 cross-sectional study found that higher perceptions of a fitness influencer’s expertise corresponded to an increase in users’ intentions to engage in physical activity, highlighting the influence of professional credentials in shaping public behavior [30]. In response to concerns about the psychological effects of unregulated fitness content, a 2023 study developed a two-stage audit tool to assess the credibility of popular Instagram fitness accounts, finding that fewer than half met criteria for credibility [31]. This demonstrates how structured oversight and appropriate auditing systems can strengthen credibility and public trust.
National dermatologic societies, such as the AAD, Women’s Dermatologic Society (WDS), and the American Society for Dermatologic Surgery (ASDS), are well-positioned to oversee accreditation, building on their existing infrastructure for continuing medical education (CME) and professional standards [19]. Centralizing governance and auditing panels within these societies would reinforce legitimacy and ensure credibility. To encourage dermatologist participation within these governing societies, solutions could include awarding CME credit for accredited digital content creation or verification, institutional recognition of digital scholarship, and expanding malpractice policies to cover digital communication. These incentives could reduce the burden on dermatologists and make participation in accreditation more feasible [23-27]. Funding could be supported through a combination of professional society resources, industry partnerships with dermatologist-approved skincare brands, and philanthropic or federal grants focused on digital health literacy. The AAD’s ongoing advocacy efforts on a federal level have already shown efforts in payer policy reversals and reimbursement denials [32], underscoring how this organization shows promise and authority in continuing to advocate for the specialty in various domains, including digital discourse. For instance, one study evaluated the use of artificial intelligence bots to accurately identify and respond to posts on Reddit containing dermatology misinformation, using automated responses based on AAD guidelines [33]. This model highlights the central role of professional societies like the AAD in content verification and patient education online, reinforcing these societies’ suitability to lead a professional digital accreditation effort.
Content verification is another core element of a physician-governed accreditation system. Stepwise verification protocols, ideally led by board-certified dermatologists affiliated with the above societies, could be used to evaluate content for clinical accuracy and alignment with evidence-based dermatology guidelines. This process may include an initial review, periodic audits, and real-time monitoring to rapidly identify and address misinformation or misleading content. Artificial intelligence tools could supplement this process by detecting potential misinformation in real-time and flagging it for expert review. While it has limitations, preliminary findings suggest that automated systems can accurately identify and respond to misinformation [21,33]. This supports their potential integration as tools for dermatologist-guided fact-checking.
Transparency is another key component of this accreditation framework. Accredited users, especially skinfluencers, would be required to disclose financial relationships, brand partnerships, and conflicts of interest with skincare brands, pharmaceutical companies, or related advertisers, with visible verification markers distinguishing them from non-medical influencers. It would signal to other social media users that the content they are viewing adheres to dermatologist-approved standards, distinguishing the user from other non-medical influencers disseminating misinformation. Collaborations with platforms, as seen in YouTube’s 2022 Health Initiative [34,35], could help integrate accreditation markers into platform search algorithms, increasing visibility of credible dermatology voices.
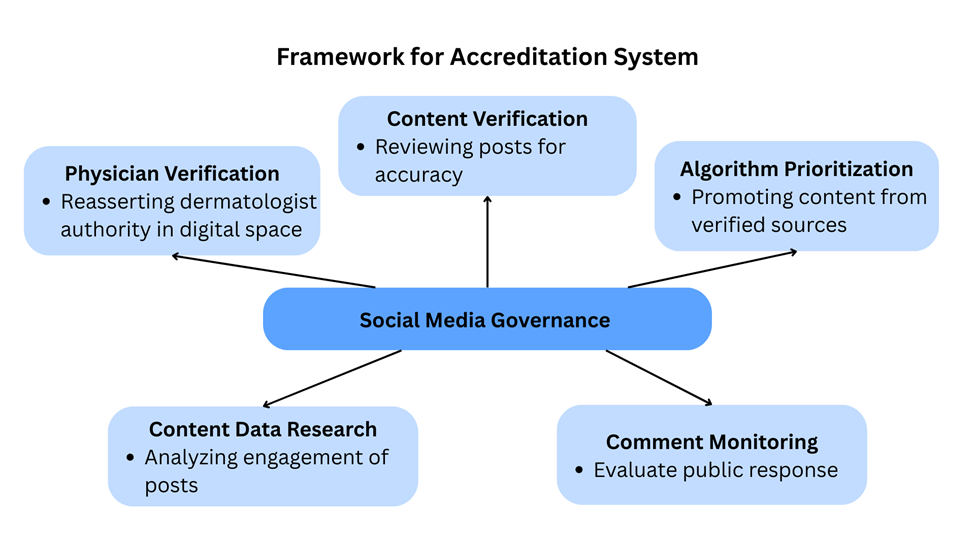
Together, governance, verification, and transparency provide a conceptual foundation for a scalable physician-governed accreditation framework to combat the growing challenge of dermatologic misinformation online (Figure 2). It does so by establishing expert-led oversight, real-time content verification, mandatory transparency, and partnerships with social media platforms. Such a system can reinforce dermatologists’ expertise and central role in shaping online skin health communication.
Figure 2. Conceptual framework for a physician-governed social media accreditation system.
Impact on Public Health
Dermatologists are uniquely positioned to make a meaningful public health impact through digital platforms by sharing accurate, evidence-based skin health education. Surveys show that a majority of patients seek dermatology information online before consulting a dermatologist, preferring medically accurate, physician-provided dermatology information over anecdotal or influencer-driven content [36,37]. Studies of YouTube and other platforms demonstrate that videos with the greatest number of likes or highest ratings contained subjective, misleading, and unscientific claims, while higher quality videos had fewer positive ratings [11,38]. These findings suggest a disconnect between patient preference for trustworthy medical information and the prevalence of misleading content, highlighting the critical need for structured intervention. An accreditation system built into major social media platforms could help bridge this critical gap by clearly redirecting audiences toward trustworthy dermatology sources and empowering individuals with the knowledge to make informed decisions. In doing so, social media and the internet serve as influential tools not just for communication, but for public health promotion and disease prevention.
Importantly, a physician-governed accreditation model could also reduce disparities in access to reliable information. Vulnerable populations include adolescents, individuals with skin of color, and those with limited access to specialty care; these populations are most exposed to misinformation and at risk for making healthcare decisions based on this. For instance, in one study, patients expressed a notable desire for more “professional content on YouTube,” “opportunities to chat with providers,” and “online consultations” [36]. Meeting these patients’ expectations can impactfully strengthen the physician-patient relationship, improve information continuity between online and clinical settings. A recent survey by the American Society for Dermatologic Surgery reported that social media ranked among the top three factors that influence skin care product purchase, citing that 41% of patients reported following current or potential healthcare providers on Instagram [39]. An active focus on inclusivity and equitable access to credible dermatology information can help prevent unintended consequences of marginalizing community-based voices and safeguarding medical validity in various types of communities. This approach aligns with broader literature on digital health equity, which stresses how accessible online health communication helps reduce disparities in patients [40,41]. Studies have shown that patients welcome the expansion of online consultations and digital access to professional dermatologic information, which could lower costs, expand access to care, and improve convenience for patients and dermatologists alike [36,42].
Beyond advancing public health, a physician-governed accreditation system could offer significant advantages for dermatologists by helping them reclaim visibility and reassert professional authority in the digital landscape. Aside from clearly distinguishing themselves from non-expert voices online, a credible digital presence may create new professional opportunities, including product collaborations, industry partnerships, research initiatives, media appearances, and speaker invitations at academic or public events [43]. Through accreditation, dermatologists can leverage social media not only as a tool for patient outreach but also as a platform for professional development and leadership within the specialty.
Ultimately, accreditation has the potential to shift digital dermatology discourse from a significantly unregulated influencer economy toward a system rooted in public health, medical ethics, and transparency. Standardization of how dermatologic information is communicated and shared online would improve the overall quality, transparency, and consistency of health content accessible to the public. By amplifying and increasing accessibility to evidence-based information, the framework could help redefine social media as not just a marketing or communication tool, but as a scalable, regulated public health resource with the capacity to improve dermatologic outcomes on a global scale.
Challenges and Ethical Considerations
Efforts to implement standardized, physician-led regulatory frameworks for dermatology-related information on social media platforms face both logistical and ethical challenges. One obstacle is resistance by major social media platforms to external oversight. Currently, no platform utilizes physician-led oversight. While some platforms adopted fact-checking to monitor the accuracy and credibility of health content, as seen with YouTube’s Health initiative [34,35], other platforms have scaled back these efforts, leaving misinformation less regulated. For example, in 2025, Meta, which owns Facebook, Instagram, WhatsApp, and Messenger, announced the discontinuation of its fact-checking program in the United States, shifting towards a community-based “notes” model [44]. This policy change in content moderation policies raises concerns about the feasibility of implementing physician-led accreditation across multiple platforms.
Regulation of dermatology-related misinformation also raises complex ethical considerations. Stricter verification systems could inadvertently censor non-physician educators, especially those from underrepresented or underserved communities. Individuals from these backgrounds often lack access to specialty care and rely on social media as a source of health information. Community content creators frequently provide accessible, culturally attuned dermatologic advice. For instance, culturally embedded hair practices, especially among individuals with skin of color, have become normalized or embraced using social media [45]. Limiting these voices might reduce diversity of perspectives and further marginalize populations that already systematically face barriers to dermatology care. Similarly, heavy reliance on fact-checking mechanisms introduces the risk of bias in determining what counts as credible health information. The background, degree of education, and values of those performing verification inevitably impact which content is flagged or prioritized. Furthermore, with an increase in artificial intelligence (AI), there is an increased risk of AI-generated misinformation circulating unchecked without adequate transparency. To address this, social media platforms should also implement clear labeling standards and audit AI-generated content for accuracy and bias.
To address these challenges, various types of safeguards may be integrated into the accreditation framework. To help ensure inclusive representation, oversight and auditing panels should include diverse stakeholders, including dermatologists, patient advocates, community-based creators, and digital media experts. Partnerships between dermatologists and high-reach, non-physician influencers can also broaden access to credible, evidence-based content without excluding marginalized or community-based creators. Sustained investment in community engagement, algorithm transparency, and collaborative governance can help foster an online ecosystem where both content accuracy and representation coexist.
Future Directions
The development of a physician-governed social media accreditation model remains conceptual and would require rigorous evaluation before widespread implementation. Future research efforts should examine both the feasibility and impact of this system through a wide range of methods. Randomized controlled trials can assess whether accreditation markers improve the audience's ability to identify credible dermatology content or influence behavioral outcomes, such as improved adherence to evidence-based skincare practices or reduction in the use of harmful, unnecessary treatments. Survey studies could be used to evaluate public perceptions and user preferences toward physician-endorsed content compared to unverified skinfluencer content. Additionally, platform-based pilot programs could serve as preliminary models for integrating accreditation, providing real-world insights into scalability. Pilots can consider being platform-specific (e.g., Instagram, YouTube, TikTok) or content-specific (e.g., product/treatment reviews, skincare routines, tutorials) to determine which format would benefit more from structured oversight. Collaborations with technology companies could enable preliminary testing of the accreditation system within search or recommendation algorithms. Collectively, these efforts would allow for refinement, identification of logistical challenges, and assessment of user engagement with accredited content. This data can also be presented to policymakers and lawmakers, facilitating the development of updated standards for responsible digital health communication.
CONCLUSION
Dermatology’s inherently visual nature and close relevance to skincare and aesthetics, which is increasingly popular in digital discourse, make it susceptible to misinformation on social media, while also positioning the specialty in particular to lead innovative solutions. This literature review outlined the rationale, feasibility, and conceptual framework for a physician-governed accreditation system designed to prioritize clinical accuracy, transparency, and patient safety in digital dermatology communication. Such a model could help patients more reliably identify credible sources while addressing gaps in existing platform-based interventions. By integrating dermatology-specific expertise with digital health regulation, this framework has the potential to contribute meaningfully to emerging discourse on digital health governance and the role of dermatologist leadership in shaping the digital landscape.
ACKNOWLEDGEMENTS
None.
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest.
REFERENCES
- Fox S. (2011). Social Media in Context. Pew Research Center. Available at: https://www.pewresearch.org/internet/2011/05/12/social-media-in-context/
- Nguyen M, Youssef R, Kwon A, Chen R, Park JH. (2021). Dermatology on TikTok: Analysis of content and creators. Int J Womens Dermatol. 7(4):488-489.
- Concilla A, Laughter MR, Presley CL, Anderson J, Rundle CW. (2022). The Dermatologist on Social Media: When the Pros Outweigh the Cons. Comment on "Risks and Benefits of Using Social Media in Dermatology: Cross-sectional Questionnaire Study". JMIR Dermatol. 5(1):e31943.
- We let everyone know. (2025). No one knows skin, hair, and nails like a dermatologist. (n.d.). Available at: https://www.aad.org/member/publications/impact/2025-issue-1/your-dermatologist-knows
- Magin P, Pond D, Smith W, Watson A. (2005). A systematic review of the evidence for 'myths and misconceptions' in acne management: diet, face-washing and sunlight. Fam Pract. 22(1):62-70.
- Finnegan P, Murphy M, O'Connor C. (2023). #corticophobia: a review on online misinformation related to topical steroids. Clin Exp Dermatol. 48(2):112-115.
- Ward S, Rojek N. (2022). Acne Information on Instagram: Quality of Content and the Role of Dermatologists on Social Media. J Drugs Dermatol. 21(3):333-335.
- Freemyer B, Drozd B, Suarez A. (2018). A cross-sectional study of YouTube videos about atopic dermatitis. J Am Acad Dermatol. 78(3):612-613.
- Ranpariya V, Chu B, Fathy R, Lipoff JB. (2020). Dermatology without dermatologists? Analyzing Instagram influencers with dermatology-related hashtags. J Am Acad Dermatol. 83(6):1840-1842.
- Villa-Ruiz C, Kassamali B, Mazori DR, Min M, Cobos G, LaChance A. (2021). Overview of TikTok's most viewed dermatologic content and assessment of its reliability. J Am Acad Dermatol. 85(1):273-274.
- Pithadia DJ, Reynolds KA, Lee EB, Wu JJ. (2020). A cross-sectional study of YouTube videos as a source of patient information about topical psoriasis therapies. J Dermatolog Treat. 31(4):366-369.
- Iglesias-Puzas Á, Conde-Taboada A, Aranegui-Arteaga B, López-Bran E. (2021). "Fake news" in dermatology. Results from an observational, cross-sectional study. Int J Dermatol. 60(3):358-362.
- Kaňková J, Binder A, Matthes J. (2025). Health-Related Communication of Social Media Influencers: A Scoping Review. Health Commun. 40(7):1300-1313.
- Sundelson AE, Jamison AM, Huhn N, Pasquino SL, Sell TK. (2023). Fighting the infodemic: the 4 i Framework for Advancing Communication and Trust. BMC Public Health. 23(1):1662.
- Kai-Cheng Y, Francesco P, Pik-Mai H, David A, Christopher T-L, John B, et al. (2021). The COVID-19 Infodemic: Twitter versus Facebook. Big Data & Society. 8 (1):205395172110138.
- Smith AJ, Hachen S, Oquendo MA, Bhugra D, Ventriglio A, Liebrenz M. (2024). A cross-sectional study of policies from American medical organizations about public communications from physicians in the digital age. Scientific Reports. 14(1):29566.
- Farnan JM, Snyder Sulmasy L, Worster BK, Chaudhry HJ, Rhyne JA, Arora VM, et al. (2013). Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 158(8):620-627.
- Ethical Physician Conduct in the Media. (n.d.). (2025). Available at: https://code-medical-ethics.ama-assn.org/ethics-opinions/ethical-physician-conduct-media#:~:text=Protect%20patient%20privacy%20and%20confidentiality,may%20lead%20to%20potential%20conflicts
- American Academy of Dermatology (2018). Position Statement on Medical Professionalism in the Use of Social Media. Available at: https://server.aad.org/forms/policies/Uploads/PS/PS-Medical%20Professionalism%20in%20the%20Use%20of%20Social%20Media.pdf
- Greenberg R, Fallon-Friedlander S, Lieblich L, McBurney E, Resneck J. (2006). Ethics in medical practice: with special reference to dermatology. Am Acad Dermatol. Available at: https://server.aad.org/Forms/Policies/Uploads/AR/COE%20-%20Ethics%20in%20Medical%20Practice%20Booklet.pdf
- Lanius C, Weber R, MacKenzie WI Jr. (2021). Use of bot and content flags to limit the spread of misinformation among social networks: a behavior and attitude survey. Soc Netw Anal Min. 11(1):32.
- Xu S, Kwa M, Lohman ME, Evers-Meltzer R, Silverberg JI. (2017). Consumer Preferences, Product Characteristics, and Potentially Allergenic Ingredients in Best-selling Moisturizers. JAMA Dermatol. 153(11):1099-1105.
- De Angelis G, Wells GA, Davies B, King J, Shallwani SM, McEwan J, et al. (2018). The use of social media among health professionals to facilitate chronic disease self-management with their patients: A systematic review. Digit Health. 4:2055207618771416.
- DeCamp M, Koenig TW, Chisolm MS. (2013). Social media and physicians' online identity crisis. JAMA. 310(6):581-582.
- Militello M, Yang RA, Anderson JB, Szeto MD, Presley CL, Laughter MR. (2021). Social Media and Ethical Challenges for the Dermatologist. Curr Dermatol Rep. 10(4):120-127.
- Arimany Manso J, Taberner Ferrer R, Pidevall I, Mascaró Ballester JM, Martin-Fumadó C. (2020). Use of Photography in Dermatology: Ethical and Legal Implications. Actas Dermosifiliogr (Engl Ed). 111(2):107-114.
- Chretien KC, Kind T. (2013). Social media and clinical care: ethical, professional, and social implications. Circulation. 127(13):1413-1421.
- Boyer C, Baujard V, Geissbuhler A. (2011). Evolution of health web certification through the HONcode experience. Stud Health Technol Inform. 169:53-57.
- Metzger MJ, Flanagin AJ, Eyal K, Lemus DR, Mccann RM. (2003). Credibility for the 21st Century: Integrating Perspectives on Source, Message, and Media Credibility in the Contemporary Media Environment. Annals of the International Communication Association. 27(1):293-335.
- Wang L, Li X, Wang D, Zhu J. (2024). Influence of social media fitness influencers' credibility on users' physical activity intentions. Digit Health. 10:20552076241302016.
- Curtis RG, Prichard I, Gosse G, Stankevicius A, Maher CA. (2023). Hashtag fitspiration: credibility screening and content analysis of Instagram fitness accounts. BMC Public Health. 23(1):421.
- Bridges AG, Werpachowski N. (2025). Advocacy and Compliance Issues Impacting Dermatology in 2025. Cutis. 115(6):188-190.
- Sager MA, Kashyap AM, Tamminga M, Ravoori S, Callison-Burch C, Lipoff JB. (2021). Identifying and Responding to Health Misinformation on Reddit Dermatology Forums With Artificially Intelligent Bots Using Natural Language Processing: Design and Evaluation Study. JMIR Dermatol. 4(2):e20975.
- Health Y. (2022). YouTube announces certification programme for health-related channels. Available at: https://health.youtube/
- ETHealthworld.com. (2022). YouTube announces certification programme for health-related channels. Available at: https://health.economictimes.indiatimes.com/news/industry/youtube-announces-certification-programme-for-health-related-channels/95126512
- Gantenbein L, Navarini AA, Maul LV, Brandt O, Mueller SM. (2020). Internet and social media use in dermatology patients: Search behavior and impact on patient-physician relationship. Dermatol Ther. 33(6):e14098.
- Ross NA, Todd Q, Saedi N. (2015). Patient seeking behaviors and online personas: social media's role in cosmetic dermatology. Dermatol Surg. 41(2):269-276.
- Mueller SM, Jungo P, Cajacob L, Schwegler S, Itin P, Brandt O. (2019). The Absence of Evidence is Evidence of Non-Sense: Cross-Sectional Study on the Quality of Psoriasis-Related Videos on YouTube and Their Reception by Health Seekers. J Med Internet Res. 21(1):e11935.
- Boen M, Jerdan K. (2022). Growing impact of social media in aesthetics: Review and debate. Clin Dermatol. 40(1):45-48.
- Jones M, DeRuyter F, Morris J. (2020). The Digital Health Revolution and People with Disabilities: Perspective from the United States. Int J Environ Res Public Health. 17(2):381.
- Koehle H, Kronk C, Lee YJ. (2022). Digital Health Equity: Addressing Power, Usability, and Trust to Strengthen Health Systems. Yearb Med Inform. 31(1):20-32.
- Fogel AL, Sarin KY. (2017). A survey of direct-to-consumer teledermatology services available to US patients: Explosive growth, opportunities and controversy. J Telemed Telecare. 23(1):19-25.
- Benabio J. (2013). The value of social media for dermatologists. Cutis. 91(6):269-270.
- Joel K. (2025). More Speech and Fewer Mistakes. Meta. Social Technology Company. Available at: https://about.fb.com/news/2025/01/meta-more-speech-fewer-mistakes/
- O'Brien-Richardson P. (2021). "Mane"taining: How Black Adolescent Girls Maintain Their Cultural Hair Practices in Physical Education Class. J Phys Act Health. 18(8):981-987.
 Abstract
Abstract  PDF
PDF